Plantar fasciitis is the most common source of running-related heel pain. Understanding how the plantar fascia becomes irritated lets you calm the inflammation quickly and adjust training so the condition does not linger for months.
01What Is Plantar Fasciitis?
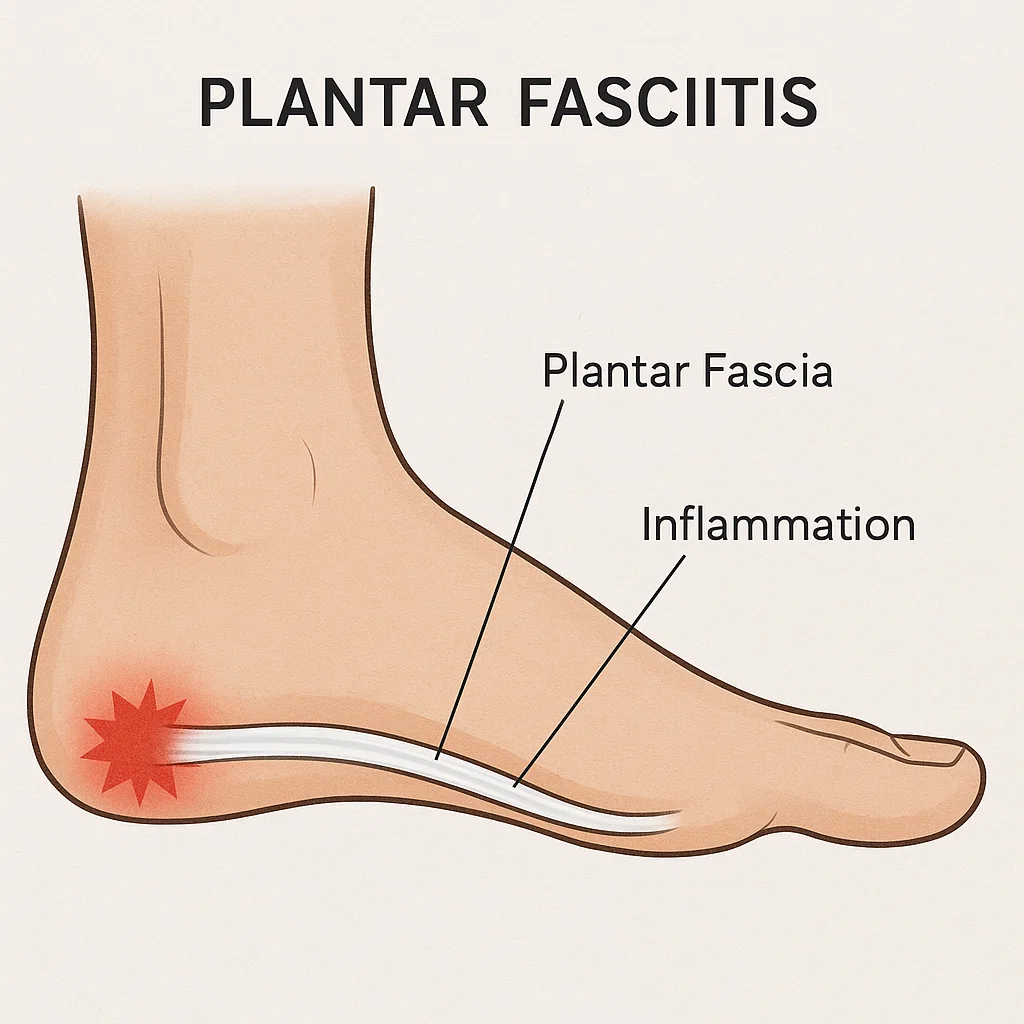
The plantar fascia is a thick band of connective tissue running from the heel bone to the toes. It supports the foot’s arch and stores elastic energy each time you load the foot. Plantar fasciitis describes microtears and irritation within that tissue where it anchors to the heel.
Typical symptoms include sharp, stabbing pain under the heel when taking first steps in the morning, discomfort after prolonged standing, and tenderness when pressing near the medial heel. The condition is usually mechanical overload rather than an inflammatory disease, but persistent strain keeps the tissue in a sensitised state.
02Why It Develops
- Rapid increases in mileage, hill work, or speed sessions that overload the plantar fascia before it adapts.
- Running in worn-out shoes or footwear with insufficient arch support for your stride.
- Limited ankle dorsiflexion or calf tightness that shifts extra strain to the fascia.
- Weak intrinsic foot muscles and glute control that allow the arch to collapse.
- Long hours standing on hard surfaces between training sessions.
03Treatment & Relief
Heel pain rarely resolves from rest alone. Combine short-term relief techniques with gradual loading to rebuild tissue tolerance:
- Modify training: Reduce running volume and intensity temporarily, but maintain fitness with cycling or deep-water running.
- Morning mobility: Perform towel stretches, ankle circles, and calf mobilisations before taking the first steps each day.
- Manual care: Roll a frozen water bottle or lacrosse ball along the arch for 5–10 minutes to desensitise painful tissue.
- Ice & anti-inflammatories: Short bouts of ice massage or over-the-counter NSAIDs like ibuprofen can calm pain for a day or two, but they do not repair the fascia—use only as directed by your clinician.
- Strength progression: Start with seated calf raises and short-foot exercises, progress to single-leg calf raises and heavy slow resistance.
- Night splints or taping: Use them for short stints if first-step pain remains intense.
Foam rolling the calves and plantar fascia can ease muscle tension and improve ankle motion, yet lasting recovery still depends on gradually loading the tissue.
See a clinician if heel pain lasts longer than two weeks, you experience numbness, or you cannot bear weight.
04Long-Term Prevention
- Rotate running shoes and replace them every 300–500 miles to maintain cushioning.
- Keep calf strength and ankle mobility work in your routine twice per week.
- Gradually build long runs and hill sessions by no more than 10% per week.
- Include foot doming, toe spreading, and balance drills to reinforce arch control.
- Resume full training only when you can walk briskly and hop pain-free.
Consistent foot care makes plantar fasciitis far less likely to return once symptoms settle.
05Footwear to Use & Avoid
Running shoes act like shock absorbers and guides for how your foot lands. During recovery, the right model can unload the plantar fascia while the wrong pair keeps tugging on the heel.
Lean on these designs
- Moderate stability shoes: Models with gentle medial support or guidance rails stop the arch collapsing without forcing your motion.
- Cushioned daily trainers: Fresh foam underfoot dampens repetitive impact so the fascia can calm down.
- Rockered midsoles: Slightly curved soles help you roll through toe-off with less strain on the plantar attachment.
- Custom orthotics or insoles: Add them if a clinician has prescribed arch support specific to your foot mechanics.
Skip these for now
- Minimalist shoes: Ultra-flexible, zero-drop models demand high calf and foot strength you may not yet have during rehab.
- Super-light racing flats: Thin midsoles transmit ground force straight to the heel.
- Worn-out trainers: Compressed cushioning and stretched uppers reduce support exactly when you need it most.
- Stiff carbon-plated shoes: The rigid toe spring can increase leverage on a sore plantar fascia unless you are racing pain-free.
Aim for a smooth ride that feels supportive but comfortable—your best shoe is the one that lets you walk and jog without the fascia flaring afterwards.
Last updated: October 9, 2023
Disclaimer: This article is educational and not a substitute for personalised medical advice. Consult a healthcare professional for diagnosis and treatment.